Verification and validation are design controls required by the FDA to ensure the medical devices you manufacture are safe, effective, and fit the intended use. Often, they happen in combination, with verification occurring during the medical device design process and validation happening at the end. This article reviews the similarities and differences between the two processes so that you can make sure your quality management system remains FDA compliant.
What are verification and validation?
Verification is a quality control process that checks whether your design meets the specifications you laid out in your product development specification (PDS). When you verify your medical device design, you will typically review design documents, conduct inspections, and perform bench testing. In short, you are verifying the design outputs match the design inputs and that your processes produce the correct product.
Validation, on the other hand, is a process that checks if the device or components fulfills the intended use and user requirements. Validation typically involves evaluating the finished device to see if it meets the user requirements, such as biocompatibility. In short, you are validating that your medical device works as intended.
What happens during verification?
During verification, you and your development team analyze the design and confirm it matches the design inputs outlined in the PDS. Verification activities may involve reviewing design documents, conducting inspections of the product and product processes, and performing bench testing. Verification can happen throughout the design process, including design reviews, FMEA, code reviews, and bench testing. Before manufacturing your device, you want to ensure each design input has a corresponding design output.
What happens during validation?
During validation, you test your device or component, checking that it functions correctly and meets user requirements outlined in the PDS. Validation activities include evaluating the product in real-world or operating environments such as functional, performance, stress, load, compatibility, interoperability, and usability testing. Validation occurs at the end of the development process because the results confirm your medical device is ready for manufacturing.
What are the differences between verification and validation?
While verification and validation are related, they are different activities with different goals and are typically performed at separate times during the development process. There are five main differences between verification and validation these are:
- Purpose: Verification proves the manufacturing process produces the correct product. Validation proves that the product works as intended.
- Timing: Verification is typically performed during development, while validation happens after product development.
- Methods: Verification occurs through reviews, inspections, and bench testing that do not involve real-world testing. Validation involves using the product and evaluating its performance in a live environment.
- Output: Verification activities produce outputs such as review and inspection reports. Validation activities produce outputs such as test and acceptance reports.
- Responsibility: Verification is typically the development team’s responsibility, while validation is the responsibility of an independent testing group.
Let us look at a standard surgical stapler for a real-world example of the differences. At a rudimentary level, the stapler must fit comfortably in a surgeon’s hand and reliably fire staples in succession into tissue. Verification involves test-firing staples into a simulated tissue or foam to show that the stapler functions as designed. Validation tests that the stapler works in an operating room while being used by a surgeon on human tissue.
What are the FDA requirements for design verification and design validation?
The Food and Drug Administration (FDA) has specific medical device design validation and verification guidelines that all medical device manufacturers operating within the United States are legally required to satisfy. These guidelines fall under the design controls portion of current good manufacturing practices (cGMPs) outlined within the Code of Federal Regulations (CFR).
Verification, as defined by the FDA, is “confirmation, through the provision of objective evidence, that the requirements for a specific intended use or application have been fulfilled.” In short, the FDA requires confirmation by objective evidence that design output meets design input. With verification activities such as mechanical and electrical bench testing and tissue testing, you prove to the FDA that all your internal processes make the correct product. You can also identify and correct issues early in the development cycle.
According to the FDA, design validation involves “establishing documented evidence which provides a high degree of assurance that a specific process will consistently produce a product meeting its predetermined specifications and quality attributes.” This means manufacturers must prove that the device specifications conform to the intended use and user needs. With validation activities such as clinical trials, and biocompatibility testing, you prove to the FDA that all your external processes make the correct product. You can also find and correct issues verification cannot identify.
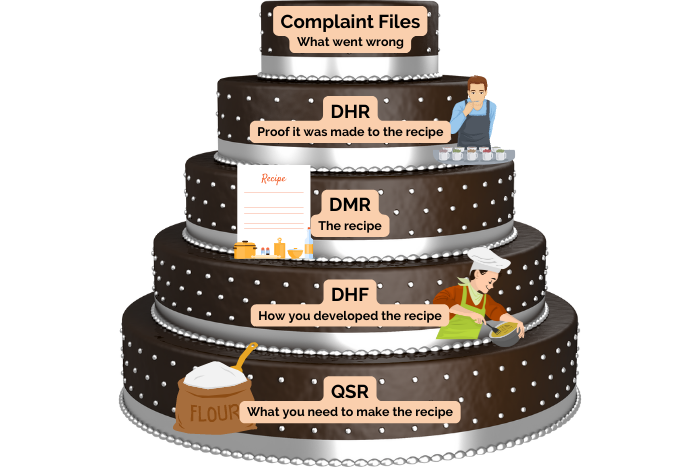
The FDA requires that medical device manufacturers document validation and verification and that the documentation is available for review during inspections. The FDA also requires that you conduct validation and verification activities systematically and scientifically. Any results of these activities must be documented and stored within your design history file (DHF).
In addition to these requirements, the FDA has specific guidance on validating and verifying computer systems. This includes software used in manufacturing the product, systems used to collect, process, and report data, and those used to control critical production processes.
Most importantly, neglecting or underperforming validation and verification can result in defects or failures, causing injury, illness, or even death. If that were to happen, you could face costly issues such as recalls, lawsuits, damage to your company’s reputation, and poor customer satisfaction. In addition, your medical device may not be approved for sale by the FDA. Given how much time and money goes into medical device development, failure to gain FDA approval would result in significant financial loss.
How do you verify a medical device?
Medical device verification guarantees that devices are designed and implemented correctly and meet the necessary standards and regulations set by the FDA. The steps involved in performing verification of a medical device include:
- Identify the device requirements by reviewing your PDS and other relevant documents to determine what requires verification.
- Develop a verification plan that outlines the scope, objectives, and approach for the verification process. In addition, your verification plan should specify the verification methods, the criterion used, and any resources and personnel needed.
- Review the design documents, such as technical specifications and drawings, to see if they match the design inputs outlined in the PDS.
- Conduct inspections of the manufacturing and assembly process.
- Perform walkthroughs of the medical devices’ design and performance.
- Perform a static analysis of the device. Static analysis is a means of debugging involving testing the medical device against the requirements.
- Evaluate the device’s design and implementation against ISO and FDA regulations.
- Analyze and document by creating reports or other documentation to summarize the results of the verification activities. You are required to store the results within the DHF following the FDA’s record requirements.
How do you validate a medical device?
In the medical device industry, validation is particularly important to confirm that the device is safe, effective, and fit for its intended use. The steps involved in performing validation of a medical device include:
- Identify the validation requirements by reviewing your PDS and other relevant documents to determine what requires.
- Develop a validation plan outlining the validation process’s scope, objectives, and approach. In addition, your validation plan should specify the methods and criteria used, as well as the resources and personnel needed.
- Conduct functional testing to confirm that your medical device functions as intended.
- Conduct performance testing to see if your medical device can withstand the intended use and environment.
- Evaluate the device in a live operational environment, such as clinical testing, to confirm it performs as expected under normal conditions.
- Analyze and document the results of the validation process. You will need to store the reports within the DHF.
In conclusion, design verification and design validation activities are an important part of medical device design controls required by the FDA. These processes can help identify and assess risks and address them before they cause damage or harm to the end user. As a result, proper verification and validation lead to improved safety, quality, and customer satisfaction. If you need help performing verification and validation or would like expert advice on navigating the regulatory process, contact us, we would be happy to help.
Get a Free Quote
About Synectic Product Development: Synectic Product Development is an ISO 13485 certified, full-scale product development company. Vertically integrated within the Mack Group, our capabilities allow us to take your design from concept all the way to production. With over 40 years of experience in design, development, and manufacturing, we strive for ingenuity, cost-effectiveness, and aesthetics in our designs. Learn more about our medical device design services and see how we can help your next project.